Advance care planning information for clinicians
What matters most to consumers and their whānau should be at the centre of care planning and delivery.
These pages provide staff working in health care with the tools, training and support to develop the skills, confidence and systems to achieve this goal.
Evidence shows consumers and their whānau want open, honest communication from their health care team, but receive this to varying degrees. We can support consumers to make better treatment and care choices by including what is important to them, their values, preferences and goals into the decision-making process. Advance care planning is one way we can do that.
Order resources
We have a suite of advance care planning tools and resources to help people think about and document what matters most to them.
Digital PDFs of our advance care plans, guides and brochure are available here.
Clinicians can order My advance care plan & guide booklets here.
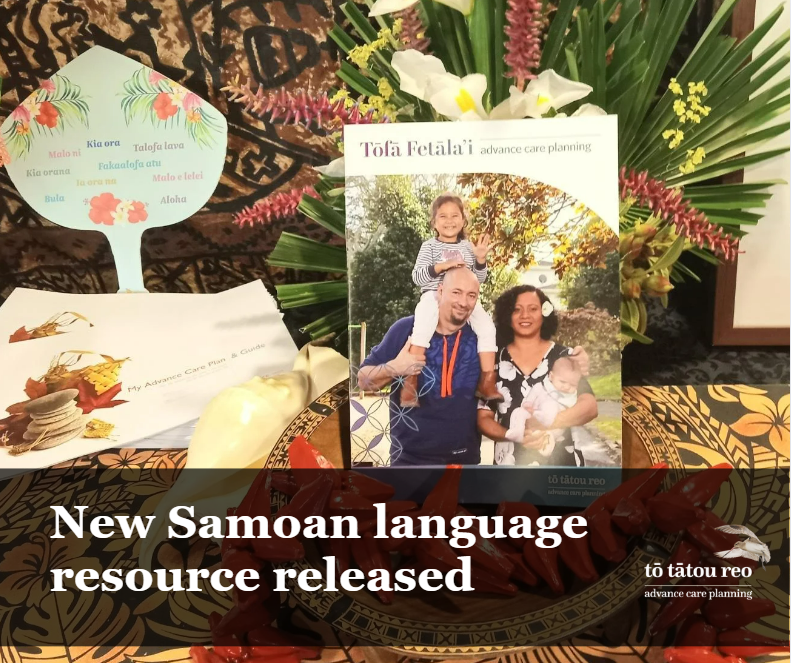
Small quantities of Whenua ki te whenua and Tōfā Fetāla’i advance care planning booklets can be ordered here.
Clinician news and events
About advance care planning
Advance care planning is the process of thinking about, talking about, and planning for future health care and treatment. Advance care planning is a person/whānau-led process and there are a number of different ways a person and their whānau might want to do this (for example, at a marae, with whānau, with their clinical team, alone or with other members of their community). It is important the health care team supports them in that process.
-
• what really matters to them, their values, priorities and goals
• their current and possible future health
• the care and treatments they might need
• the choices they might face.
-
• their whānau about what matters most to them and what they would want if their health changed or they were unable to tell us themselves
• their general practice team and other health care providers about their current and future health, treatments and care options they might face and to understand the risks and benefits
• health care providers when their health changes and they need to make decisions about treatment(s).
-
• so everyone knows what care would support what is most important to them
• for treatments and care they would or would not want if their health changes
• the treatments they do not want if they are unable to speak for themselves.
-
• informing us about who should be involved in decision-making
• providing information about a person’s values, goals and preferences to inform treatment planning
• providing direction about what a person would want should they be unable to tell us themselves, including advance directives.
An overview of advance care planning in Aotearoa New Zealand
In New Zealand, advance care planning is a process. The focus is on understanding what is important now and in the future. This video gives an overview of the advance care planning process including the tools available to support this work.
Advance care planning is not just about end of life care and treatments
It is the process of empowering consumers to participate in their health care planning and deciding what treatment and care best meets their values, goals and preferences now and in the future.
An advance care plan captures what is important to the person and outlines the care and treatment they would want if unable to communicate for themselves.
Shared goals of care discussions are a part of the advance care planning process. These discussions are with a person and/or their whānau about the goals of care for a specific admission to hospital, aged residential care or long term care facility.
The Serious Illness Conversation Guide Aotearoa supports clinicians to have conversations with seriously ill people and their whānau, including shared goals of care discussions.
Shared decision-making in health care is complex and when it does not go well it causes harm to consumers and their whānau. The video exploring how the way we work impacts consumer experience explores what consumers experience when shared decision-making does not go well and what clinicians think might contribute to it.
Benefits
Advance care planning, including shared goals of care, has benefits for the person and their whānau, health care staff and for the health care system.
-
• Encourages conversations about what is important to a person and their whānau.
• It can help people feel more in control, reduce anxiety and fear and can positively enhance a person’s hope in the face of progressive illness.
• Advance care planning has shown to increase a person’s understanding of their condition, improve their comfort, and reduce stress, anxiety and depression for whānau after a person dies.
-
• Helps develop relationships between a health care team and the person/whānau.
• By taking the time to sit with a person/whānau and gain an understanding of who they are, what is important to them, what they are hoping for and what they might be worried about, can create and support a genuine connection
-
• Allows end-of-life wishes to be known and followed.
• Evidence from local and international studies has found that advance care planning supports a substantial reduction in unwanted and unwarranted treatments for consumers. This leads to measurable reductions in hospital length of stay, hospital costs and emergency admissions in the last year of life, with a corresponding increase in consumer satisfaction and quality of life. Systems have not always encouraged the consumers’ voice to drive the care delivery model. For some, this has led to inequitable access to services, unwarranted and unwanted treatments; and culturally unsafe and inappropriate experiences.
• Advance care planning provides a model where the cultural framework and beliefs, values, hopes and goals of the person and their whānau are central to care and treatment planning. The consumers’ voice can be most easily heard when systems view advance care planning as a service, not a project.
What clinicians can do
1. Create your own advance care plan.
2. Prepare yourself to have conversations with consumers by:
– considering your biases
– ensuring you have the skills and confidence.
3. Have conversations with the person and their whānau.
4. Document the person’s goals, values, preferences and advance directives.
5. Use what matters most to the person and whānau in care planning and delivery.
6. Promote advance care planning:
– to the person and their whānau
– within your team or organisation
Related resources
• Saving your electronic ACPlan for record keeping and sharing
• Advance care plans, guides and brochures are available online here
• My advance care plan & guide booklets can be ordered here
• Download the five year strategy as PDF or Word doc
• Advance care planning 101 presentation and guidelines for use:
The presentation is designed to be delivered to health care staff who don’t have a great deal of knowledge about advance care planning. It can, and should, be adapted for the audience you are presenting to. If all the content is presented as it is, it will take approximately an hour. There are also guidelines about how to deliver the presentation. See documents below:
Advance care planning 101 presentation | Guidelines for using the advance care planning 101 presentation